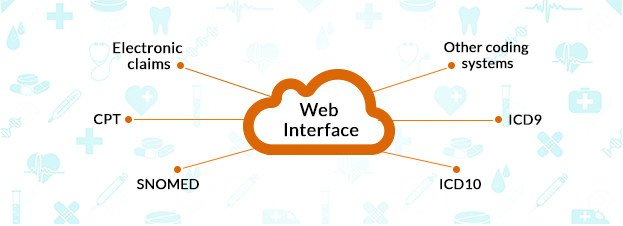
Healthcare IT Experts has developed Billing systems for seamless claim processing with automatic claim generation and processing after creation of encounters. This system provides web interface to complete all the required details for creating electronic claims, utilizing ICD9, ICD10, CPT, SNOMED, and other coding systems.
The system is integrated with different clearing houses, and payer companies and integration settings are facility based, according to their existing channel or network. The system is highly effective to process primary, secondary and tertiary claims and process ERAs for calculations of patient’s responsibilities.
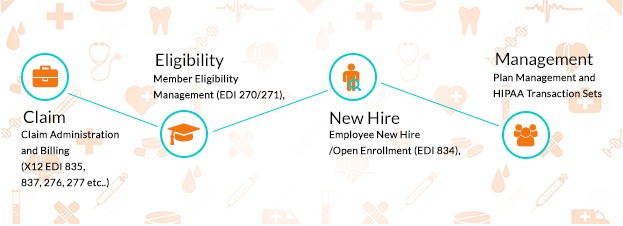
Our system takes care of the following transactions:
- Claim Administration and Billing (X12 EDI 835, 837, 276, 277 etc.)
- Member Eligibility Management (EDI 270/271)
- Employee New Hire /Open Enrollment (EDI 834)
- Benefit Plan Management and HIPAA Transaction Sets
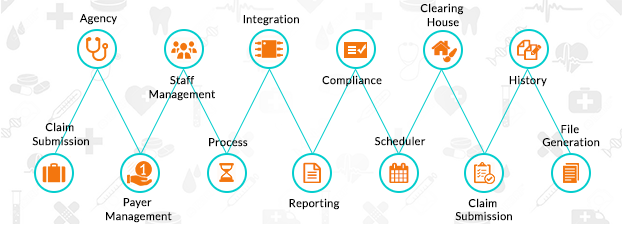
The main features involved in our developed system are:
- Agency (clinical and financial records)
- Agency Staff Management and access mechanism
- Payer Management (multiple payer and private pay)
- Claim Submission
- Integrated assessment
- Reporting and analysis
- Automated IDT Process
- Clinical history maintenance
- Scheduler
- HIPAA Compliance
- Claim Submission
- EDI File Generation
- Integration with Clearing House